Healthcare Reform: Sure-Fire Impacts for Nurses

Healthcare Reform Proposals are just that: proposals. The rhetoric is largely political, with Democrats in daily disagreement with Republicans—no surprise there. Despite President Obama's urgency, the actual final draft of a fully realized Healthcare Reform proposal could take weeks to iron out. In the interim we are treated to daily howlings that illustrate the diversity of perspective. How do the current proposals potentially impact the Nursing Industry AND are nursing voices being heard on Capitol Hill?
The most vital healthcare issues include:
- 50 million Americans without health insurance
- Millions more underinsured
- Exclusion of individuals with pre-existing medical conditions from mainstream health insurance
- Financial waste in Medicare and Medicaid
- Nursing shortage
- Escalating Healthcare Costs vs. alarming drops in Quality of Care
Some of these are sure to be addressed with a sweeping healthcare reform bill, but how the expanse of the final reforms will ultimately affect the nation's nurses is still unclear.
In the meantime, is it possible to forecast a few positive repercussions the Nursing industry will, undoubtedly, feel?
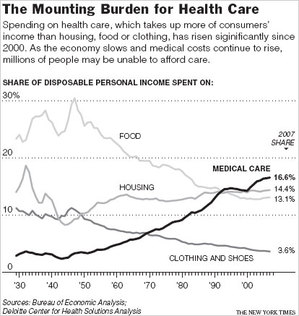
*Source, NYTimes
What Keeps Nurses Up At Night
Beyond the wider healthcare issues lies Nurses' perspective on these problems:
- Lack of affordable health insurance is keeping nearly 50 million Americans arm's length from preventative care and wellness
- More and more patients are presenting in critical and emergent medical situations thanks to lack of regular doctor and nurse care, driving demand for intensive and costly care
- Lack of money is straining hospitals and other facilities that then must scale back staffing levels, leaving nurses working at full-speed over the long-haul
- Lack of adequate nursing staff is making for unsafe working conditions for nurses, repercussions in patient outcomes and quality of care
- Lack of nurse retention strategies amplifies need for new nurses
- Lack of money, innovation, and facilities has been detrimental to producing nursing faculty capable of training new nurses and Advanced Practice nurse forces.
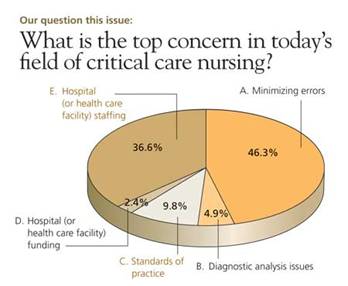
*Source, Johns Hopkins University, School of Nursing, “Second Opinion”
How HC Reforms are Sure to Impact Nurses
If nothing else, the surest Healthcare reform will certainly offer some degree of relief to uninsured Americans. President Obama, along with a vocal force of lawmakers, politicians, and advocacy groups, supports a public health insurance program. The overall gist: uninsured individuals should be given the right to join a low-cost government-sponsored insurance program should they so choose.
Since cost is impeding preventative care for many, it makes sense that once a pathway to low-cost healthcare is greased that many, will of course, take advantage. Nurses across the board would be indirectly relieved….
- Staffing headaches would improve
- Education for new and experienced nurses would likely have new financial juice pumped into its withers
- Nurse Advocacy would continue to improve Nursing clout.
Nurse Advocacy is Actively Improving
Already an impact is being realized in organizations committed to nursing advocacy. Urgency to draw attention to the role nurses play at every level of healthcare is being felt and the healthcare reform dialog is spurring this onward.
Read the major media reports on current healthcare reform. Many of them continue to portray the main decision-makers in healthcare as: doctors/physicians, pharmaceutical companies, and insurance companies. But things have turned critical and many lawmakers know insurers—major financial lobbyists-- may not get the upper hand in this tussle.
 Less recognized but increasingly vocal front-line stakeholders include nurses, nursing homes and long-term care organizations, rural physicians and nurses, and certainly patients of all kinds and from every region.
Less recognized but increasingly vocal front-line stakeholders include nurses, nursing homes and long-term care organizations, rural physicians and nurses, and certainly patients of all kinds and from every region.
**Impact: Leaders from some of the leading nursing associations have participated in recent healthcare reform dialog at the White House. Powerful nursing voices have come from the American Academy of Nurse Practitioners (AANP), the American Nurses Association (ANA), and the American College of Nurse Midwives (ACNM). The AARP, one of the most respected and powerful consumer advocacy groups—representing millions of Baby Boomers—has been extra vocal in support of Healthcare Reform that includes underscoring the now and future role of Nursing in healthcare delivery. Raised in unison and with a singular message, finally nurse-friendly decision-makers at the top of government are in a position to support and strengthen nursing's future role.
Easing the Workload in Patient Care: Safe Staffing
Healthcare reform that makes care available to uninsured Americans will, given time, lessen the workload on nursing. While it may not be immediate relief, the trickle-down is a sure thing. But the problem is no longer completely centered on the uninsured. Lack of hospital funding and a vacillating nurse shortage—thanks to a quicksand economy-- are two major pieces of the puzzle confounding nurse staffing.
 Guess what? Nurse staffing levels are a cornerstone to quality of care, which in turn sculpts patient satisfaction, which also, in turn, quickly and keenly drives hospital reputation up or down….(1) Who in this economy can afford for their BRAND to take a beating?
Guess what? Nurse staffing levels are a cornerstone to quality of care, which in turn sculpts patient satisfaction, which also, in turn, quickly and keenly drives hospital reputation up or down….(1) Who in this economy can afford for their BRAND to take a beating?
To harried RNs the term is “staffing level,” a.k.a. working short, burned-out, sick of it, and “over it.” Only in the larger more political arena does it get bandied about as WORKFORCE. The dope is this: the number of nurses staffing various patient care areas has been stretched thin wherever possible and necessary, making day-to-day long-term nursing practice uncomfortable, even painful in some cases. Phrases like “Mandatory Overtime,” “Unsafe Staffing Levels,” and “Nursing Workforce Safety,” are commonplace in nursing administration realms. Still, what does this have to do with Healthcare Reform?
Many nurses and nurse advocacy groups would love nothing more than to see mandatory nurse-patient ratios written into any national health reform agenda. President Obama, formerly Senator Obama-IL, endeared himself to just these issues while serving the State of Illinois.
The staffing issue goes neatly hand in hand with patient care: the more equitable the nurse-patient ratio, the safer and more quality the patient care, and the happier the patient and family.
The staffing problem is so primal to nurses that corps of them, unionized in some regions, are aggressively stalking the beast:
In Pennsylvania nurses recently celebrated a victory when they leveraged lawmakers there to establish firm mandatory nurse-patient staffing ratios based on type of patient care unit, acuity, and a few other measurable variables.(2)
A popularly cited study on nurse staffing levels reveals that “each additional patient per nurse was associated with a 7% increase in the likelihood of dying within 30 days of admission and a 7% increase in the odds of failure-to-rescue.” The findings in this study also dovetailed to nurse job satisfaction, proof to nurse managers and hospital administrators who must regularly wrestle with nurse retention challenges. (3)
Key to the current reform is patient care, regardless of how the chips finally fall.
Any nurse of any kind and at any educational level knows that his or her job rests on patient care and advocacy.
The Preventative for Preventative Healthcare….
President Obama aggressively supports the deployment of a public insurance system that may be used to provide health insurance coverage to those Americans without insurance or to those with too little.
Emergency Care and Critical Care: The Real Nursing Cost
Thanks to high healthcare costs driving a growing population of uninsured Americans, fewer are engaged in real preventative healthcare. In this recent economic crisis Emergency Departments, some already strangled with patients, are hemorrhaging staff, facilities/beds, and money. Safety net providers like these are logging increasing numbers of uninsured patients, many newly unemployed and now uninsured.(4)
In many states where communities have low-cost urgent care clinics designed to provide practical alternatives to EDs, resources are spent. For example, in Greensboro, North Carolina the region is facing just such a burdensome problem: low-cost community clinics established to provide support for the area EDs are jammed with increasing numbers of uninsured customers/patients, many of whom cannot be served in these facilities. (5)
The very sick that present emergently are often admitted and transported to Critical and Acute Care units, even Surgery, where nurse to patient ratios are much smaller and care is costly and intensive. In an ideal healthcare system, in which access to preventative care is convenient and sensible for all, this type of worst case care could be headed off at the pass, patient after patient, with regularly scheduled preventative visits to a primary care physician or, better yet, an independent Nurse Practitioner. Throw in reform that also guarantees access to affordable prescription drugs and you may have some real relief to squawk about.
*Impact: Nurse staffing levels, affected by the volume of very sick and/or emergent uninsured patients—can clearly be seen as a burden most likely to ease in a system that finally offers a low-cost public insurance coverage option to the near 50 million uninsured Americans.
Will The Promised Financial Juice Finally Be Pumped Into Nursing Education?
 The educational pathways for nurses are weak at best—totally dilapidated at worst. The ingredients in this brew are culled from funding problems (no money for more nurse educators, teaching facilities, or preceptor sites), human resource fallacies (under-estimating how much mandatory over-time and low-staffing levels overworked nurses could STAND before they ditch), antiquated pink-collar job discrimination (general lack of proper salary or incentives for nurse faculty who remain primarily female and mid-career), and overall slow progress (nursing schools are quickly launching quite sophisticated online nursing programs, pushing accelerated degrees for career-changers, and trying out innovative tactics like shared curriculums, teaching sites, and increasing pay for nurse faculty).
The educational pathways for nurses are weak at best—totally dilapidated at worst. The ingredients in this brew are culled from funding problems (no money for more nurse educators, teaching facilities, or preceptor sites), human resource fallacies (under-estimating how much mandatory over-time and low-staffing levels overworked nurses could STAND before they ditch), antiquated pink-collar job discrimination (general lack of proper salary or incentives for nurse faculty who remain primarily female and mid-career), and overall slow progress (nursing schools are quickly launching quite sophisticated online nursing programs, pushing accelerated degrees for career-changers, and trying out innovative tactics like shared curriculums, teaching sites, and increasing pay for nurse faculty).
You could say that nurse education has already been financially impacted.
Part of the American Recovery and Reinvestment Act of 2009 included $500 million earmarked to medical education, including nursing. Also promised money-- the National Health Service Corps and medically underserved community health clinics. Early reports are that millions of these stimulus dollars have already have been rushed to truss up nursing school programs and expand services at underserved clinics. (6) Also, HR 1460, Nurses' Higher Education and Loan Repayment Act of 2009, was introduced as a new (pending) Bill in March 2009. (7)
*Source, Oncology Nursing News
Nursing education is a multi-pronged issue:
- We need embattlements of new nurses to serve as front-line patient caregivers
- We simultaneously need new and inspired Nurse Educators to lead the forces
- We hope experienced RNs will continue to show enthusiasm for the rich opportunities in Advanced Practice.
Opportunities Improve for Advanced Practice Nurses
 Since emphasis is clearly being planted on shaping a more financially streamlined Healthcare system you might begin to imagine how deployment of Advanced Practice Nursing forces able to leap tall buildings with a single bound AND provide lower-cost care-- throughout Healthcare--, could help fortify reform efforts AND slash costs for facilities as well as patients. (8)
Since emphasis is clearly being planted on shaping a more financially streamlined Healthcare system you might begin to imagine how deployment of Advanced Practice Nursing forces able to leap tall buildings with a single bound AND provide lower-cost care-- throughout Healthcare--, could help fortify reform efforts AND slash costs for facilities as well as patients. (8)
Nurse Practitioner median annual salary: $82,590
Family Practice Physician median annual salary: $159,228 (Salary.com)
But only when legislators include NPs in reform measures will real change take place. For example, the American Academy of Nurse Practitioners has urged members to appeal to legislators in writing. They urge Congress to include NPs “in the definition of primary care providers in reimbursement packages, pilots, demonstrations and stimulus packages…” (9) in order to ensure the worth of a strong and viable NP workforce that can, over time, prove to be a vital part of the healthcare solution. As of 2008, only 23 states required no “physician involvement” in an NP practice. (10)
**Impact: Expect that the value of health wellness and prevention to prevail, consequently fueling urgency for NP-Physician models or solo NPs throughout Healthcare: Adult and Women's Health, Family Practice, Rural Community Health, Neonatal, Pediatrics, Psychiatric, Gerontology, and Oncology and in facilities that include hospitals, nursing homes, rural practice and clinics, doctor's offices, VA hospitals, corrections, public schools, corporate settings, private practice, and retail clinics.
Equal Compensation for Nurse Midwives?
Cutting similar lines, the ACNM is applauding reform drafts that expand Medicare reimbursement for Certified Nurse Midwives and Certified Midwives, known as the “Equitable Reimbursement for CNMs and CMs under Medicare” (11). Up until now, CNMs have earned 35% less than physicians under the Medicare program. This disparity does a disservice to the field and in no way is reflective of the skyrocketing demand for the services of CNMs. (12)
Rural Healthcare and Rural Nursing
Already rural healthcare stakeholders are holding their collective breaths while Capitol Hill – well-heeled politicians – play verbal badminton with “healthcare reform proposals.” To rural medical personnel healthcare reforms will be the line drawn in the sand separating life and death for their patient populations. Rural doctors and nurses are fearful that any type of new reform will be more of the same, a clear forgetfulness of Rural Americans. Think these folks don't need healthcare? By the time they do, it's critical or emergent—they can't afford preventive care. (13)
Mucking up the issue of more streamlined healthcare in rural outposts-- still 24 states require documented “physician involvement” in Nurse Practitioner practice. Some of these advanced practitioners must have prescriptions approved by physicians and others must be under indirect supervision by a primary care physician, while in 23 other states NPs practice unfettered. (2008 Pearson Report)
In Minnesota the state Rural Healthcare Reform proposals include expansion of provider's roles, including Advanced Practice Nurses, to more fully utilize their “full potential.” (14)
**Impact: Rural communities will likely continue to try and bootstrap more cost-effective healthcare solutions, with or without federal help. This would surely include embracing the various Advanced Practice Nurse scopes of practice and working to find ways to collaborate meaningfully with regional hospitals and providers with viable nursing resources, as well.
 Nursing is the Fulcrum
Nursing is the Fulcrum
Most Americans at some point in their lives will be impacted by the care of a nurse. As Healthcare front line personnel they've been largely subjugated and silenced. But recent efforts to galvanize nursing have finally proven successful. Voices unified for Nursing's role in American healthcare include major nursing associations, nurse unions, and leading healthcare advocates with their own strings to pull on Capitol Hill. It goes without saying that Nursing—a Healthcare FULCRUM-- will be impacted positively by the impending Healthcare Reforms, it must be:
Staffing levels are the subject of legislative debate, patient satisfaction surveys are making and breaking hospitals, and we're all getting older and more reliant on a healthcare system that has financially outpaced most regular old Americans' financial capacities in urban, suburban, and rural frontiers.
Citations
- Nursing: A Key to Patient Satisfaction, Robert Wood Johnson Foundation,
- House Bill No. 147, General Assembly of Pennsylvania
- Hospital Nurse Staffing and Patient Mortality, Nurse Burnout, Job Dissatisfaction, Linda Aiken, Sean Clarke, Douglas Sloane, Julie Sochalski, and Jeffery Silber
- Uninsured Put a Strain on Hospitals, Reed Abelson, New York Times
- American Hospital Association, Tim Rice, Moses Cone, Greensboro, NC, YouTube
- Economic Stimulus Funding Provides Millions for Nursing Education and Jobs, Robert Wood Johnson Foundation
- H.R. 1460: Nurses' Higher Education and Loan Repayment Act of 2009
- Nurse Practitioners: The Growing Solution in Healthcare Delivery, AACN
- Health Care Reform Sample Letter, AANP
- 2008 Pearson Report, The American Journal for Nurse Practitioners
- Implementation of the Affordable Care Act, ACNM
- ACOG Endorses Full Equity for CNM(R) and CM(R) Reimbursement Under Medicare, Medical News Today
- Will Healthcare Reform Reach Rural America? , John King, CNN
- Healthcare Reform: Addressing the Needs of Rural Minnesotans, 2007
Other Sources
Policy Experts, Researchers, Hill Staffers Discuss Nursing Workforce Solutions, Center to Champion Nursing in America
Grass roots Voices Speak Up on Healthcare, The Columbus Dispatch
Providing the Nurses We Need to Improve Health Care for All Americans, AARP

